NOV. - Vol. 1, No. 3
NeuroNarratives & Holiday Cards
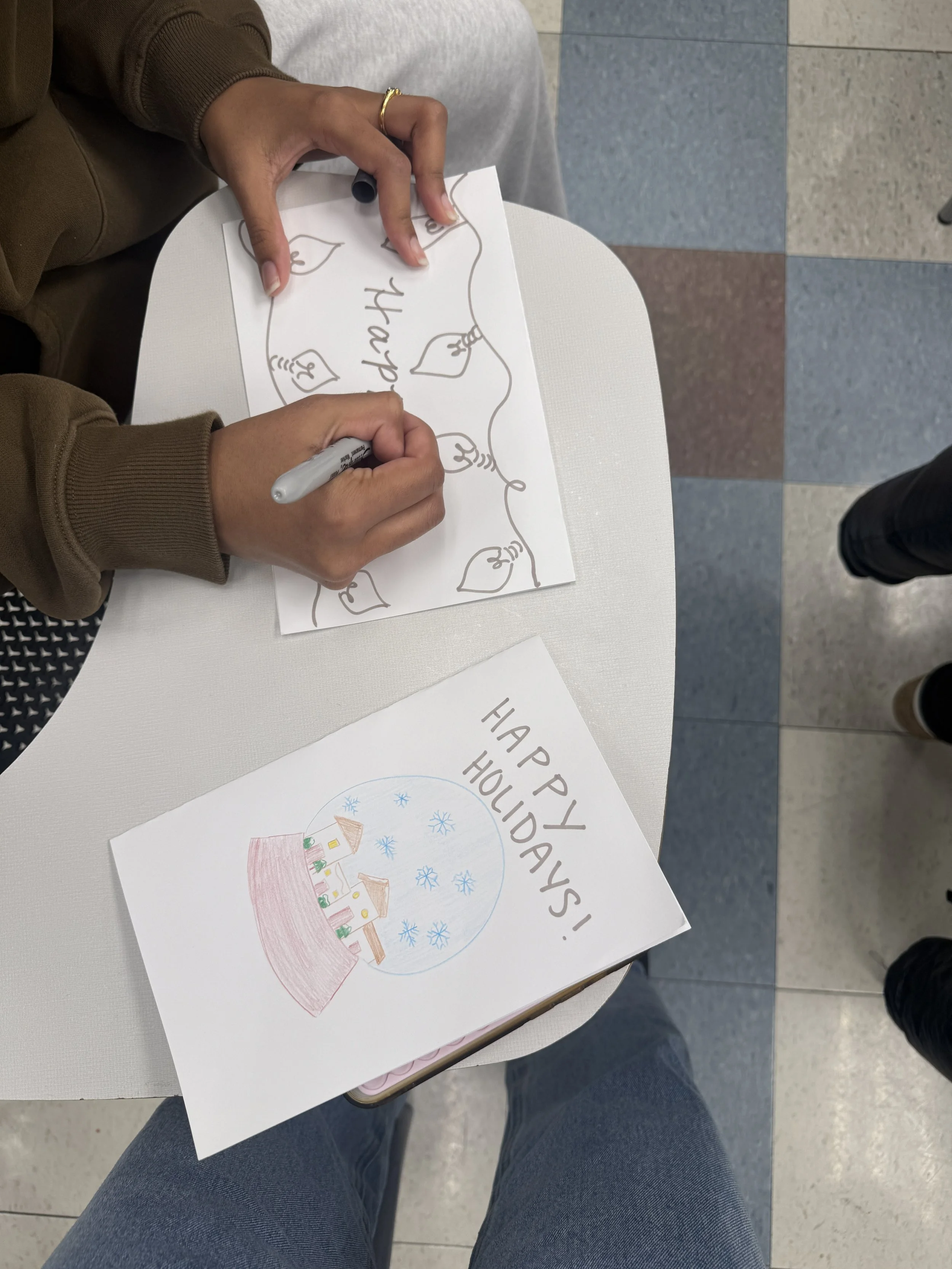
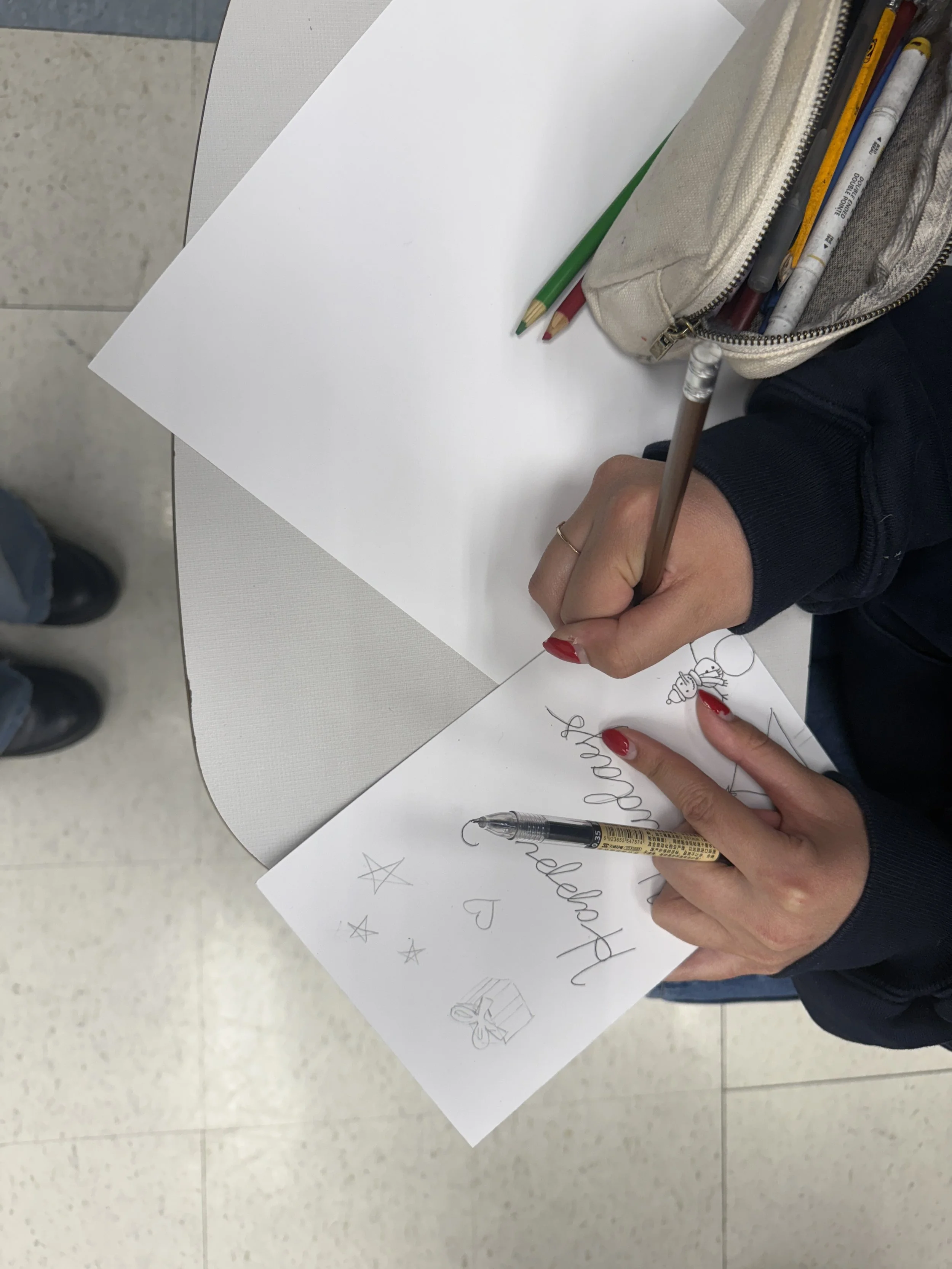
This month, the NeuroNarratives team came together to create handwritten cards for the Thanksgiving and holiday season. Each card is being shared with members of our local community and residents in senior-assisted living, many of whom are living with memory loss or spend the holidays away from family.
Our goal was simply to offer a moment of recognition and human connection during a season that is filled with both joy, but can sometimes be heavy. This work is both an act of art and an act of service, and we are grateful to everyone who joined us to bring words and creativity to paper and brighten someone’s day.
Meet Dr. Nikhil Parekh
About Dr. Parekh
Dr. Parekh brings extensive experience across public health, medicine, and integrative health. After completing his undergraduate studies, he earned his medical degree from Wayne State University and subsequently trained in epidemiology and public health. Throughout his career, he has collaborated with the federal government, led research initiatives across multiple departments, and mentored numerous students at the University of Michigan.
Abegail Byun & Dr. Parekh at the 2025 UROP Research Symposium
One of those mentees, Abegail Byun, worked with Dr. Parekh through the Undergraduate Research Opportunity Program during the 2024–2025 academic year. Under his guidance, she conducted a research project investigating integrative whole health: a patient-centered model that considers physical, mental, emotional, and social well-being. Using a Qualtrics survey of 217 participants, the project assessed wellness across eight domains.
Data analysis in RStudio revealed three major wellness profiles, highlighting how personalized approaches can improve outcomes and reduce disparities. These findings informed applications to chronic illnesses such as Alzheimer’s disease and ultimately inspired the NeuroNarratives implementation project. This research and the vision behind NeuroNarratives were recognized with a Blue Ribbon Award, underscoring its impact and meaningful contribution to community-centered health.
In direct response to these insights, NeuroNarratives was created as a community-based, interdisciplinary club. Its three-track structure—Education, Service, and Art—reflects the core needs identified in the research. By integrating science, storytelling, and art, NeuroNarratives offers a neuro-informed approach to addressing healthcare disparities, strengthening community connection, and honoring memory. The club stands as a tangible, student-led embodiment of integrative whole health principles, translating research into meaningful, sustainable action.
We thank Dr. Parekh for his dedication to compassionate, person-centered care and his passion for mentoring and educating others, and his continued support for NeuroNarratives!
Dr. Parekh x NeuroNarratives Interview
“There is a reductionist viewpoint in medicine that says that we can treat the disease but not the person, but I believe treating the individual is critical. ”
What made you interested in this area?
I grew up in a community where there were a lot of health practices that are considered to be complementary and natural. When I went to medical school I was disappointed to see that things were not often done in these ways. In clinical medicine, however, I had good mentors who were holistic in the way they approached things which encouraged me in my interests.
What is the Integrative Health system, and why is it important?
Integrative Health is composed of complementary modalities focused on wellness and treatment, emphasizing things like nutrition, spirituality, meditation, mindfulness, and yoga. It emphasizes treating the whole person instead of just that person’s symptoms, and humanizes the person within the healthcare system. Integrative Health looks at health from the perspective of the individual.
Is Integrative Health relevant to Alzheimer’s Disease?
I had a relative who was diagnosed with Alzheimer's Disease. She found comfort in, was able to connect to, and remembered a lot of things that were related to music. She even remembered me in terms of what I loved in music. She would always play music for me and remembered the music even if she didn't remember the details surrounding it. I think this is an example of how Integrative Medicine and Whole Health can impact Alzheimer's Disease; I don’t think I've seen many doctors who have asked about what their patient connects to as a person. However, as I saw with my relative, interests can be therapeutic and potential ways to understand people and treat them according to those interests.
How can Integrative Health be impactful in preventing and treating diseases like Alzheimer's
There is a reductionist viewpoint in medicine that says that we can treat the disease but not the person, but I believe treating the individual is critical. For example, after my relative developed Alzheimer's, her husband continued to take her to her music classes. We didn't understand why she could remember the music, but we knew she found peace within herself in those moments. Similarly, when an elderly relative of mine was diagnosed with Alzheimer's, faith and spiritual health were very important to her up until she passed away. If we were doing a prayer with her it had a very significant impact on her as a human being. Treating an individual based on their unique interests can be very impactful and bring peace and progress towards better health. This also goes in line with another thing I think is very important within Integrative Health, mindfulness (being aware of where you are in the present moment), which also brings peace.
If there is one thing you would like people to know, what is it?
The idea of narratives is very important. One thing I've learned on my journey in medicine is that everyone has a story. In medicine, there is a tendency to reduce our patients to the disease that they have instead of the person that they have been, are, or will be. If you are having cognitive changes, know that you still have a story. If you are a healthcare professional, know that the person who calls you at three in the morning has a story to tell. It is hard at times to remember this when you are treating thirty patients and have so many things on your plate, but it is very important.